General information
Description
The abdominal aortic aneurysm (AAA) is defined as a dilation of the abdominal aorta of at least 50% in diameter. 3cm is commonly used as cut-off value, though the clinical impact of this value remains speculative.
Classifications
By location: Infrarenal, juxtarenal or suprarenal AAA describing the proximal end.
By underlying disease: atherosclerotic, inflammatory (rare)
Incidence/Prevalence/Age dependency
2-5% of men >;60y, 6% of men >; 65y, 11% of men >; 75y
4% of women >; 65y
Affected vascular beds
Abdominal aorta
Predominant sex
Male: Female 4:1
Genetics
There is some familial aggregation with strongly elevated risk in siblings (40% males, 15% females). Rare diseases (Marfan syndrome, Ehler-Danlos syndrome) have higher associations with AAA.
Concomitant diseases
AAA in other diseases: CAD: 5-9%, PAD: 10-15%, first degree relative with AAA: 25%, elevated in obese patients >; 65y
Concomitant diseases in AAA: thoracic, iliac, femoral and popliteal aneurysms
Risk factors
Hypertension, Nicotine, COPD (?), familial predisposition
Geographical variation
[no information available yet]
Differential diagnosis
Other abdominal masses, other causes of abdominal pain or back pain.
Possible complications
Rupture, dissection, thrombosis, distal embolisations
Population screening
Topic of debate.
Symptoms and signs
The majority of patients with AAA are asymptomatic. In non-obese patients a pulsatile epigastric mass can be found. Symptoms and clues for its detection vary greatly (abdominal pain, back pain, distal embolism or ischemia (rare), signs of AAA rupture.
Diagnostic procedures
Ultrasonography is the preferred initial diagnostic test and for surveillance. CT/MRI scans should be restricted for preoperative evaluation and in cases of suspected inflammatory aneurysms. Angiography is of little value except in special cases.
Treatment/Follow up
General procedure
AAA ;5.5cm, symtomatic or rapidly expanding AAA (>;0.5cm/6 months) should undergo repair (surgical or EVAR as appropriate). For poor surgical risk patients (LVEFDiet:
Activity:
Education/Councelling:
Risk factor modification: lipid control, hypertension control
Treatment trials found to be ineffective:
Surveillance
Surveillance should be performed by ultrasonography in most cases. Optimal screening intervals remain to be determined. For smaller AAA usually yearly intervals are used, larger AAA (>;4.5-5cm) should be followed at shorter intervals (6-3 months).
Medication
[?]
Surgery
[to follow]
EVAR
[to follow]
Treatment complications
Perioperative complications: 5% MI, 6% renal failure, 1% chronic dialysis, 5-8% pulmonary failure, 1-4% peripheral microembolims, 0.5-1% ischemic colitis, 2% wound infection,
Late complications
graft infections, graft limb occlusion, complications due to additional aneurysms (thoracic, femoro-popliteal), endoleaks (EVAR)
;
Prognosis
AAA Expansion
Expansion vary greatly over time and between patients. Large aneuryms seem to have higher growth rates.
Table. Expansion rate of abdominal aortic aneurysms (after Bernstein 1984(Bernstein and Chan 1984)*).
| Initial Size of Aneurysm | No. | Mean Growth Rate | Standard Deviation | 95% CI | |
| (cm) | Pts. | (cm/yr) | (cm) | Lower Limit | Upper Limit |
|
3.0-3.9 |
32 | 0.39 | 0.8 | 0.2 | 0.57 |
| 4.0-4.9 | 35 | 0.36 | 0.9 | 0.21 | 0.5 |
| 5.0-5.9 | 32 | 0.43 | 0.84 | 0.27 | 0.6 |
| 6.0-6.9 | 11 | 0.64 | 1.24 | 0.16 | 1.1 |

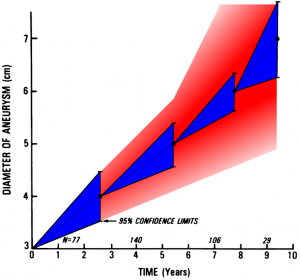
Figure. Expansion rate of abdominal aortic aneurysms. Adopted from Bernstein 1984(Bernstein and Chan 1984)*. Original (blue) based on serial echographic data from 110 patients. The blue area represents the 95% confidence interval of the mean growth rate for an aneurysm first measured at 3, 4, 5, 6cm. N-the number of patients contributing data to each segment of the mean expansion line. The red area is interpolating the highest and lowest growth rates estimated from the 3, 4, 5, and 6cm growth rate data.
To my experience, the above figure might underestimate the variability in AAA expansion rates and gives an inadequate picture of constant growth over many years, as many AAAs remain constant over several years with a sudden onset of expansion.
Risk of AAA rupture
The main determinant of AAA rupture is the its diameter. Additional factors for increased risk of rupture are diastolic hypertension, nicotine, COPD, and familial history.
Ruptured aneurysms result in 80% deaths before definitive care and 50% deaths of the remaining in hospital treatments.
